Moles and Melanoma
Advanced Mole and Skin Cancer Procedures in the San Diego Area Including Encinitas, Temecula, Rancho Santa Fe, Del Mar, El Cajon
Benign moles are referred to as “melanocytic nevi.” They appear as tan to dark brown spots or bumps on the skin, lips, and even eyes. Moles are nests of melanocytes—the pigment producing cells in the skin. Moles are present on almost every individual and develop in the first few decades of life. Moles can occur anywhere including the scalp, genital area, and mucous membranes. A birth mole is called a “congenital nevus.” Birth moles should grow proportionately with the body and be monitored regularly. Large birth moles carry a small but known risk of developing melanoma. The tendency to develop great numbers of moles runs in families. Having approximately 40-50 moles or more increases the chance of developing melanoma. Heavy sun exposure also increases the number of moles.
The ABCDEs have been developed to help patients recognize changes in moles. These changes could herald a transformation into atypical moles called “dysplastic nevi” or even melanoma. An explanation of the ABCDEs rule is explained below:
- “A” = Asymmetry:
- Moles should be symmetrical. If one side is different from the other, the mole should be investigated.
- “B” = Border:
- The border of the mole should be regular, sharp, and well-defined.
- “C” = Color:
- Uniform color should exist in the mole. More than 2 colors indicate an atypical mole.
- “D” = Diameter:
- Moles should usually be 6 mm or smaller in diameter. This is about the size of an eraser on a pencil.
- “E” = Evolution:
- New or changing moles should be examined by a physician. These changes can include changes in how the mole looks or new symptoms to the mole including itching, pain, bleeding, or ulceration.
Dysplastic Nevi
Atypical moles or “dysplastic melanocytic nevi” or “Clark’s nevi” are terms reserved for unusual moles. These moles look atypical both clinically and under the microscope. Dysplastic nevi are genetically inherited. The presence of dysplastic nevi greatly increases the risk of melanoma. Dysplastic nevi can be precursor lesions to melanoma. Individuals with 10 dysplastic nevi increase their risk of melanoma 12-fold compared to the general population (according to the Skin Cancer Foundation). Individuals with atypical moles should conduct monthly self-examinations and be examined at least annually by a dermatologist. Patients with larger numbers of dysplastic nevi should undergo a full skin examination every 6 months. New or changing moles should be evaluated and may require a biopsy to evaluate for cellular changes under the microscope.
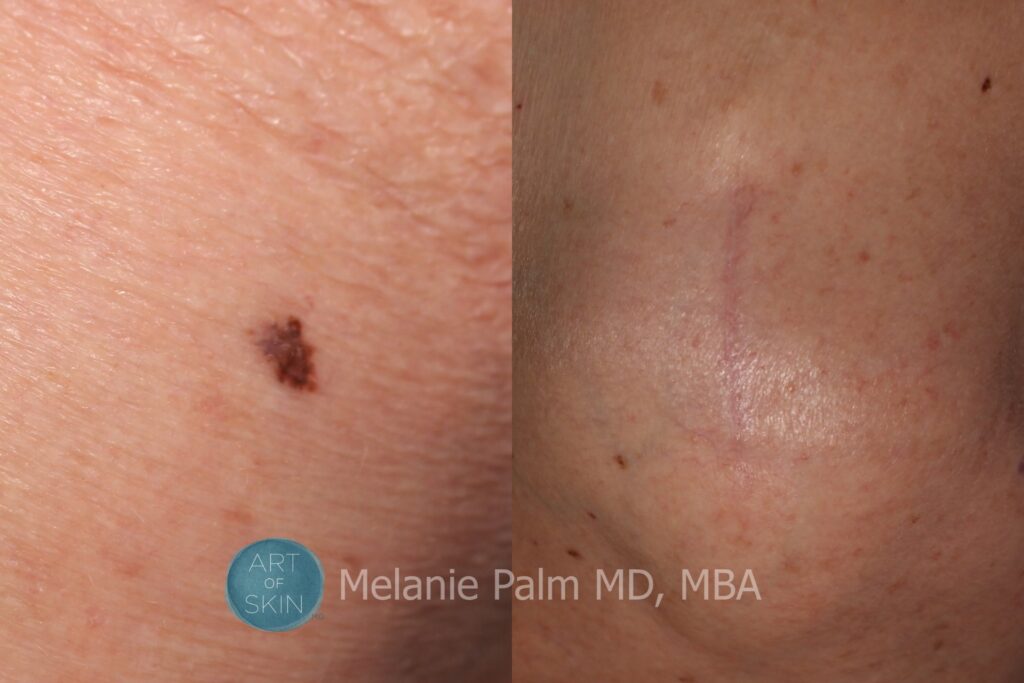
Mole Removal
If a mole is changing or is otherwise concerning, a shave biopsy may be recommended. This quick in-office procedure consists of injecting local numbing medicine and removing the affected mole. The procedure takes approximately 5 minutes and leaves a minimally detectable scar. Benign moles may either be removed by shave or surgical excision. Shave excision requires no stitches and heals by secondary intention. Surgical excision usually requires the placement of stitches. The suture line heals as a fine scar in the majority of cases.
Melanoma
Melanoma is a deadly form of skin cancer. Early detection is the key to long-term survival. In 2010, melanoma was the 6th most common form of skin cancer. Over 68,000 are diagnosed with melanoma annually. There is a strong genetic linkage to melanoma. Risk factors for melanoma include a personal history of melanoma, a first-degree relative with melanoma, a personal history of atypical moles, a history of sunburns, and light skin, hair, or eye color. UV tanning booth exposure has also been linked recently to the development of melanoma. Melanomas often appear as multicolored or very dark atypical moles. Melanomas can often be flat, although raised or nodular melanomas also occur. Amelanotic melanomas can be tan or pink in color. Melanoma can occur anywhere on the body including sun-protected areas. The palms and soles, genitalia, anus, eyes, and mouth all may develop melanoma.
Melanoma is a life-threatening diagnosis. Survival from melanoma is directly related to the thickness of a melanoma. Thin melanomas have a very high cure rate following surgical excision. Thick melanomas may metastasize to lymph nodes or other organs. Important prognostic factors from the microscopic examination of melanomas include first and foremost, the melanoma thickness (measured in mm), the presence or absence of ulceration, cellular mitoses, and lymphocytic response. The most important means of detecting a melanoma is regular skin checks. Self-exams monthly, evaluating moles for the ABCDEs, as well as an annual skin examination, are the keys to the early detection of melanoma.
If you are in the San Diego area and would like to discuss your skin cancer treatment options or would like to set up a skin cancer screening, call Dr. Melanie Palm at 858.792.SKIN (7546) to schedule your appointment.